
The Greater Manchester i-THRIVE Programme team spoke with Kim Marshall, Associate Directorate Manager for Healthy Young Minds in Heywood, Middleton and Rochdale about how the service became a top performer for NHS Benchmarking.
Download this implementation story.
Background
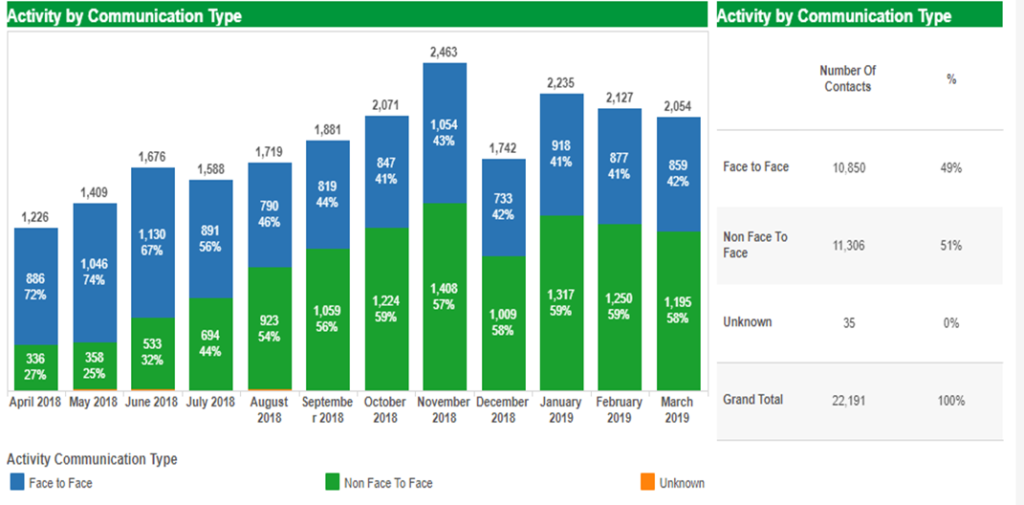
NHS England Children Young People’s Mental Health (CYPMH) access data shows how Heywood, Middleton and Rochdale (HMR) Healthy Young Minds (HYMs, a local CAMH service) is performing higher than the National Access target of 32%, with a predicted outcome of 56.9% for the year 2018/19 reporting period. This is also significantly higher than the England average of 36.1%. The service is among the NHS Benchmarking ‘Top Performers’ in a number of areas which relate to activity and recording of performance.
What approach did you take to improve access waiting time?
Kim Marshall: We took a multi-faceted approach in improving our access waiting times; initially our Clinical Director and I took a significant amount of time out of our diaries to analyse and understand why we were experiencing long wait times. The image below (see Figure 1) highlights factors that we identified to result in long waiting times within our HYMs service.
Figure 1: Factors resulting in long waiting times

We felt that it was important to understand colleague’s commitments in detail, so we interviewed all our staff, reviewed job plans and daily activities to discover actual activities. We discovered that:
- Workflows and processes were not clearly defined and staff were working above and beyond their job plans with high caseloads
- Did Not Attend (DNA) policies were not clearly defined
- Daily activities were impacting on staff wellbeing, morale and burnout
- Recruitment and retention challenges, with a number of vacant posts
- No clear ways of recording consultation and advice activities
When we had a true picture of staff daily activities, we implemented a number of changes to support staff and improve our service. Below is a list of changes we implemented:
1. New Care Pathway development
We embarked on redesigning some of our pathways, including our neurodevelopmental pathway, using the Autism Diagnostic Observation Schedule (ADOS) differently in pathways. We had an increase in routine outcome data being collected and utilised, to support quality improvement processes within the service. This was supported by having systems in place, such as supervision and case discussion in team meetings, where team and individual outcomes and any variations were discussed.
Waiting list initiatives, such as weekend clinics with case management and multi-disciplinary consultation slots, were introduced to help support staff. Incorporating the principles of the THRIVE Framework for system change (Wolpert et al., 2019) allowed for more multi-agency supervision and consultations to be offered.
Figure 2: Heywood, Middleton and Rochdale activity type
2. Clearly defined DNA processes
Increased data collection allowed us to audit our DNA rates and for this data to be used in clinical and managerial supervision to support conversations on ending treatment.
3. Supervision and consultation processes
Clearer supervision and consultation structures have been embedded within service policies. In addition, utilizing outcomes data within supervisions and team meetings ensures a consistent message is being communicated and staff effectively supported.
4. Good relationship with commissioners and stakeholders
Having good relationships with commissioners and stakeholders allowed us to address key challenges staff were facing such as not being able to accurately record their activities, including consultation sessions.
5. A well supported workforce
We have recruited to a number of vacant posts increasing staff skill mix, allowing more staff to be appropriately matched to cases. This has been supported by effective case coordination, supervision and consultation structures. Staff are being trained and supported in the principles of the THRIVE Framework through attending the i-THRIVE Academy Modules When to Stop Treatment and Getting Advice and Signposting.
Heywood, Middleton and Rochdale HYMs recently received a Greater Manchester workforce innovation fund, which allowed for the service to invest in staff wellbeing. Staff yoga and Acceptance and Commitment Therapy taster sessions were offered and staff rated these sessions to be excellent.
Image 1: Staff wellbeing session
Service improvement was really supported by colleagues having a shared value and ownership of service redesign as a whole.
How is improving access waiting times aligned with the THRIVE Framework?
Service changes and improvements in HMR HYMs are aligned with the principles of the THRIVE Framework. In line with recommendations, 60% of children and young people referred into our HYMs service are now being identified for more treatment and given the help and support they need. Those who are not, are signposted to other agencies that can better support them. For those who choose to receive an intervention, there is a clear contract and plan for children and young people in the Getting Help and Getting More Help needs based groupings, as opposed to an open-ended approach. Those who do not go on to receive further intervention, and do not require additional medical services, are signposted to additional community resources.
How have service users been affected?
The National NHS Benchmarking Report for HMR 2019, demonstrated the following:
NHS Friends and Family Test (FFT) Patient Satisfaction Score for the question ‘How likely are you to recommend to friends and family if they needed similar care or treatment?’ for HMR was 97% in comparison to the national mean score which was 88%. This suggests that the service changes and improvements made have improved the experience for children, young people and their families. As a result of the changes that have been implemented, families are getting fairer and more equitable help. Children, young people and families are kept involved in their care process, and families and referrers kept up to date on what is happening and what is planned.
Next steps
We are committed to continue to improve our service and we will continue to have team management away days to collect staff views on processes, training, how to improve data collection, recruitment, capacity progression and understand the support staff may require.
The following are key themes for further service improvement work:
- Continuing to empower staff to better support children, young people and their families.
- Utilise Sampling and Sensitivity Analysis Tools (SaSAT) skills audit data and have clear action plans to support service design.
- Conduct capacity and demand management to enable service improvement.
If you would like further information, please contact Kim Marshall at kim.marshall1@nhs.net.

Edited by the Greater Manchester i-THRIVE Programme Team and the National i-THRIVE Programme Team.
Written July 2020.